Clever RX: Getting to know your physical Clever RX card
The physical Clever RX card, it’s everywhere you want to be. Using the physical Clever RX card is a great option for many people, especially due to the lifelong habit of handing a physical card to the pharmacist. Accepted at thousands of pharmacies nationwide, read this email to learn more about what your Clever card is telling you.
The Group and Member Numbers:
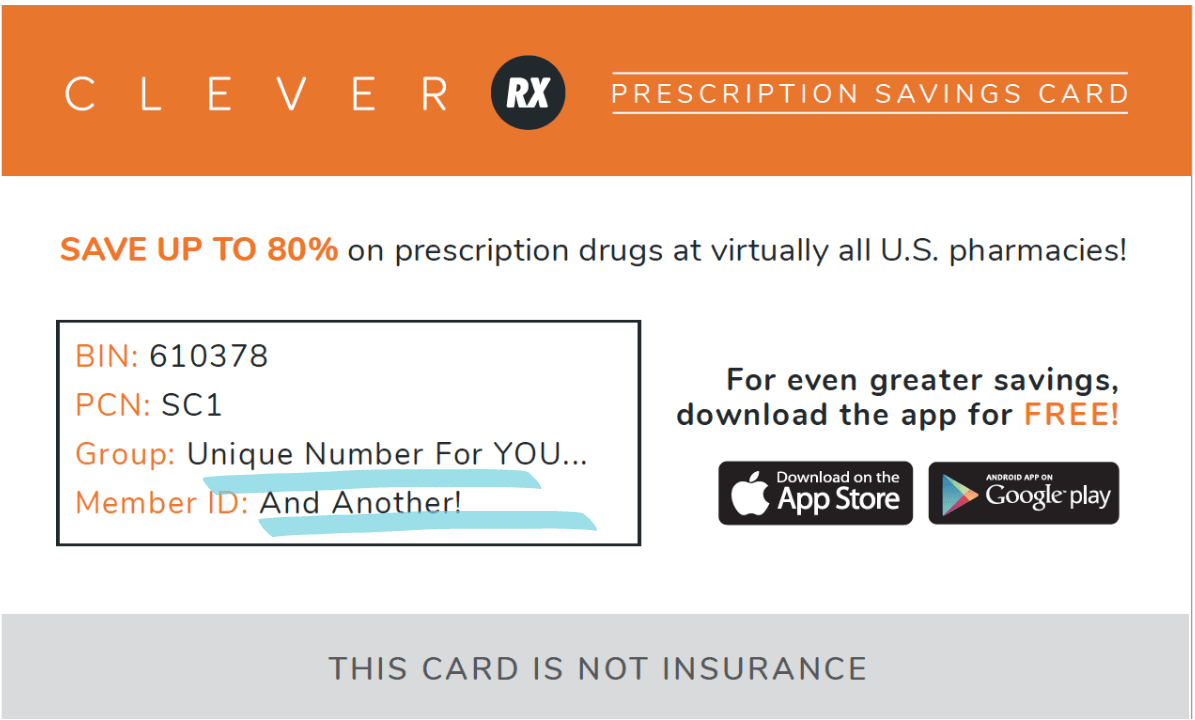
The Group and Member ID numbers on your card are how medications filled using Clever RX are tracked back to you. These numbers should be the same on every physical card you hand out and every voucher you print, text, or share. Confirm your numbers:
Group #: 3001
Member #: 1037666
Please note: If you look up a voucher on the website, there may be a “W” behind these numbers or an “A” on a voucher in the app. Have no fear, that is just how we denote the way the script was filled. It will all still be tracked back to you!
The BIN and PCN Numbers:
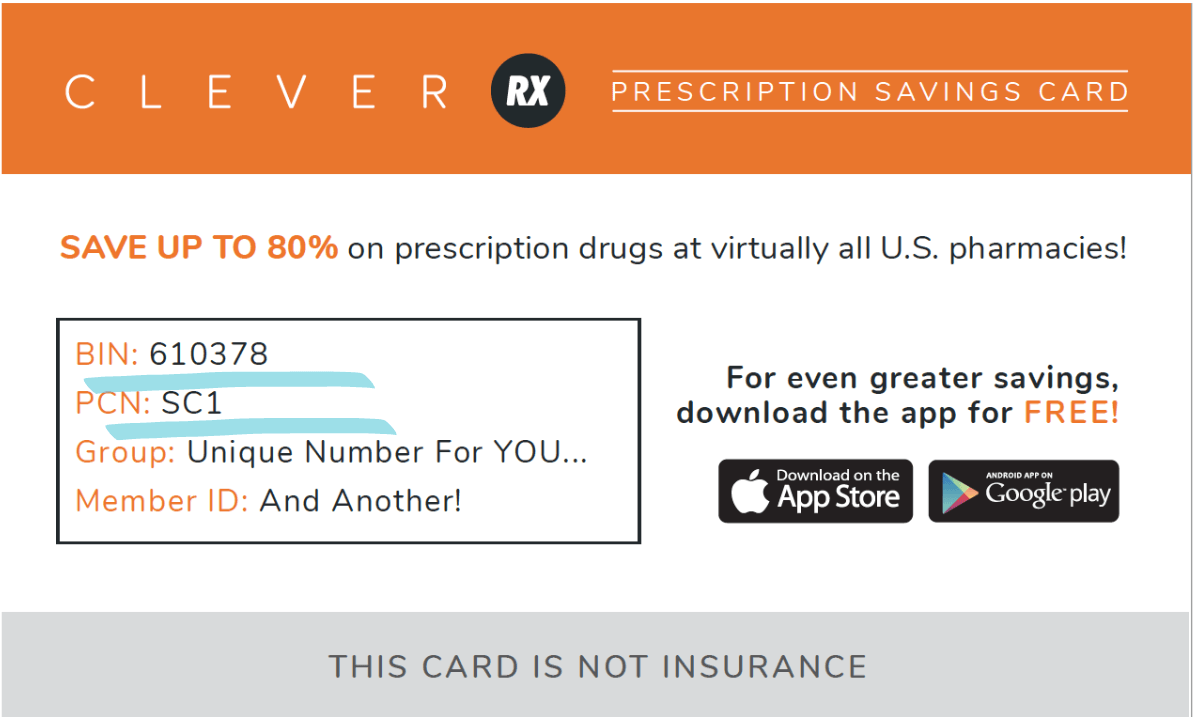
These numbers are how the pharmacist looks up the drug pricing. These numbers are NOT the same on every voucher, so no need to worry if the BIN and PCN numbers in your app or website do not match the BIN and PCN numbers on your card. Additionally, if you have purchased the alternative physical card, the BIN and PCN will be different than in the example above.
WHERE YOU CAN USE THE CARD:
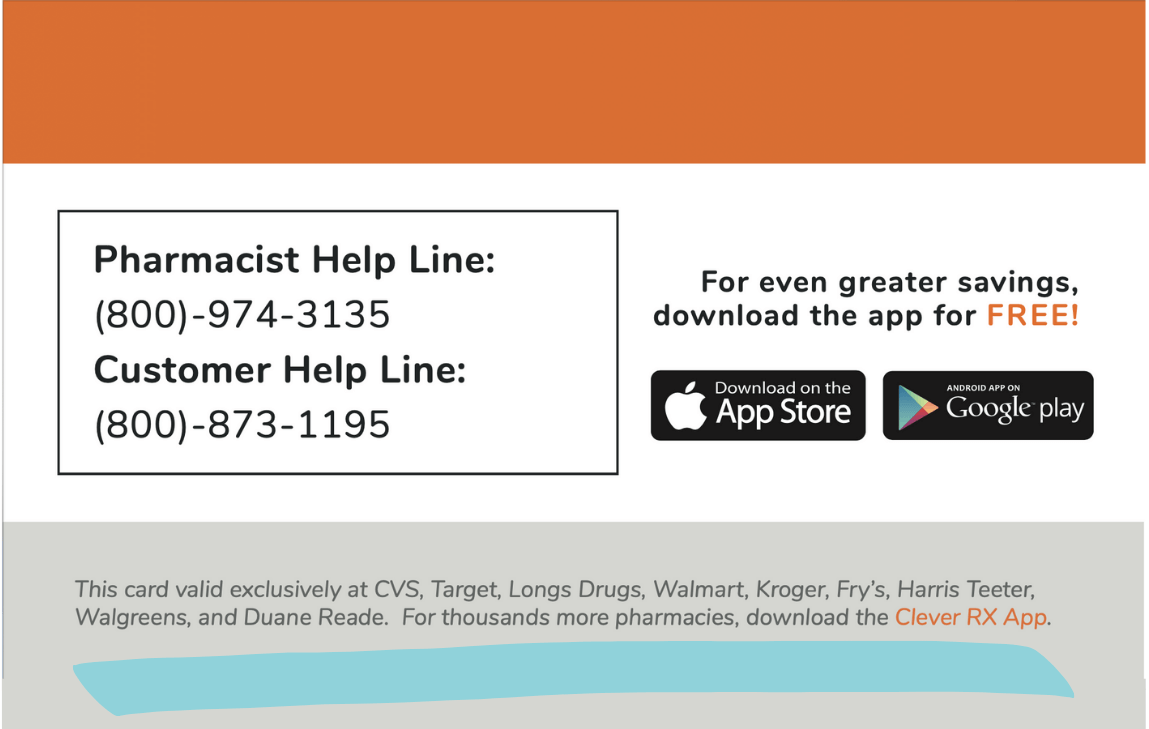
The physical Clever RX card can only be used at the places listed on the back of the card. This is VERY important, as you will be turned away if you go somewhere not listed on the card. The physical Clever RX card is accepted at tens of thousands of pharmacies across all 50 states and has our most competitive pricing at the Big 4 (Kroger, Walmart, Walgreens, CVS) . For access to all 80,000 pharmacies in our network, download, search, save, and share using the Clever RX App:
partner.cleverrx.com/Cornerstone
LEARN MORE ABOUT HOW TO USE CLEVER RX HERE
CONTACT CSM CONTRACATING DEPARTMENT TO GET APPOINTMENT WITH CLEVER RX TODAY!