WellCare: AEP is HERE
WellCare Message from 10/2/2020:
| AEP is Here! AEP is finally here, and the combination of Centene and WellCare means greater opportunity for you!
Now, you can market and sell up to 5 health plans!
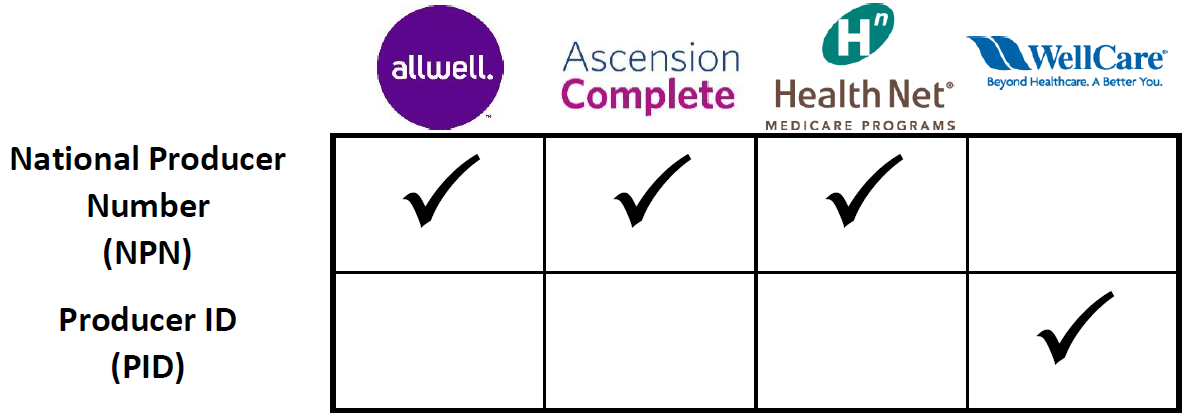
Note: Not all health plans are available in all areas. The easiest and fastest way to ensure that you are offering all plans available in your area and you are credited for each sale is to use the Ascend Enrollment Platform. (Currently, Ascend cannot be used for Fidelis Care enrollments.) Application and Enrollment Broker Identifier: It is crucial that all applications include the correct agent identifier. Ascend will automatically attach your agent identifier to each application you submit: National Producer Number (NPN), Producer ID (PID), or Fidelis Care ID. When submitting applications OUTSIDE of the Ascend Enrollment Platform, be sure to input the correct agent identifier:
*Fidelis Care Notes:
Fidelis Care does not accept paper applications. Ascend: All health plan information has been loaded into Ascend. Please note, 2021 Enrollment Applications will not be accessible until 10/15. As of 10/1 you should be able to access 2021 rates and benefits in the Ascend Mobile App. If you are not able to access 2021 plan information, please be sure to update the App. Click here for information on how to download and update the Ascend Mobile App. Warning! Beginning 10/1/2020, the WellCare Mobile Enrollment Platform and Desktop Enrollment Platform (agent assisted) will be retired and no longer accessible. You will find our 2021 plans, benefits, rates and enrollment capabilities in Ascend. Additional Resources: Click here for Application & Enrollment Tools. 2021 CMS Enrollment Guidance Policy Revisions The Centers for Medicare & Medicaid Services (CMS) has issued annual enrollment and disenrollment guidance revisions for contract year 2021. All enrollments with an effective date on or after January 1, 2021, must be processed in accordance with the revised guidance requirements. Significant Changes To Guidance:
|